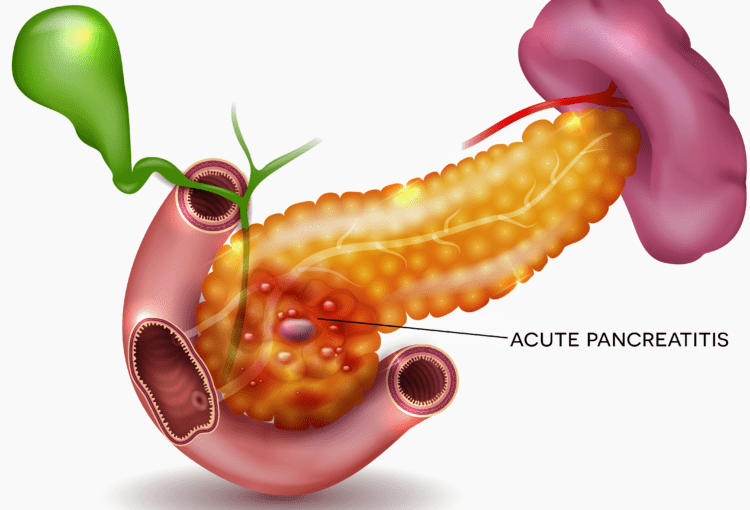
Pancreatitis, characterized by inflammation of the pancreas, can manifest as acute or chronic forms, leading to severe abdominal pain, digestive disturbances, and potential complications like diabetes or malnutrition. In modern medicine, it is often linked to factors such as gallstones, alcohol consumption, or autoimmune issues. From an Ayurvedic perspective, pancreatitis is viewed as an imbalance primarily involving the Pitta dosha, which governs metabolism, digestion, and transformation in the body. The pancreas, referred to as “Agnashaya” or the seat of Agni (digestive fire), becomes inflamed due to aggravated Pitta, often exacerbated by Ama (toxins) accumulation from poor diet, stress, or lifestyle habits. Ayurveda approaches pancreatitis holistically, aiming to pacify Pitta, eliminate toxins, restore Agni, and rejuvenate pancreatic tissues through herbs, medications, diet, and lifestyle modifications.
This article delves into Ayurvedic strategies for managing pancreatitis, with a focus on herbs and medications that target pancreatic inflammation. It is important to note that while Ayurveda offers supportive therapies, it should complement, not replace, conventional medical treatment. Always consult a qualified Ayurvedic practitioner and healthcare professional before starting any regimen, especially for serious conditions like pancreatitis.
Ayurvedic Perspective on Pancreatitis
In Ayurveda, pancreatitis aligns with disorders of the digestive system, such as “Pittashaya Shotha” (inflammation of the Pitta reservoir) or disruptions in Grahani (small intestine and pancreatic function). The root cause is often an imbalance in Pitta dosha, triggered by excessive intake of spicy, oily, or heating foods, alcohol, stress, or irregular routines that weaken Agni. Vata and Kapha doshas may also play roles in chronic cases, leading to degenerative changes (Dhatu Kshaya). Treatment emphasizes detoxification (e.g., via Panchakarma therapies like Virechana for purgation or Basti for medicated enemas), dosha balancing, and rejuvenation to reduce inflammation and prevent recurrence.
Therapies are personalized based on the individual’s Prakriti (constitution) and Vikriti (current imbalance). For instance, Pitta-dominant individuals may require cooling herbs, while those with Vata involvement benefit from grounding remedies.
Herbs and Ayurvedic Medications for Reducing Pancreatic Inflammation
Ayurveda employs a range of herbs and herbo-mineral formulations to address pancreatitis by reducing inflammation, supporting detoxification, enhancing immunity, and improving digestion. These work through anti-inflammatory, antioxidant, and Pitta-pacifying mechanisms, often by modulating cytokines, scavenging free radicals, or restoring gut flora. Below is a detailed list of key herbs and medications, their mechanisms, typical doses, and usage guidelines, drawn from clinical observations and traditional texts.
Key Herbs
– **Turmeric (Curcuma longa)**: Contains curcumin, a potent anti-inflammatory compound that inhibits pro-inflammatory pathways (e.g., NF-κB) and reduces oxidative stress in pancreatic tissues. It helps alleviate swelling and protects against further damage.
– **Mechanism**: Balances Pitta, detoxifies Ama, and supports tissue repair.
– **Dose**: 1/2 teaspoon (about 1-2 g) of powder daily, mixed with warm water or milk. For enhanced absorption, combine with black pepper or ghee.
– **Guidelines**: Take after meals; avoid high doses if on blood thinners. Consult for long-term use.
– **Guduchi (Tinospora cordifolia)**: Known as “Amrit” for its rejuvenating properties, it modulates immunity and reduces inflammation by lowering cytokine levels and balancing Pitta.
– **Mechanism**: Anti-inflammatory and hepatoprotective effects extend to the pancreas, promoting healing and toxin elimination.
– **Dose**: 500 mg to 1 g of powder or extract twice daily, as decoction or tablets.
– **Guidelines**: Ideal for chronic cases; start low to assess tolerance.
– **Triphala (Combination of Amla, Haritaki, Bibhitaki)**: A classic detoxifying formula that aids bowel regulation and reduces Ama buildup, indirectly easing pancreatic strain.
– **Mechanism**: Antioxidant properties combat oxidative damage; improves digestion to prevent inflammation triggers.
– **Dose**: 1 teaspoon (3-5 g) of powder at bedtime with warm water.
– **Guidelines**: Use for mild detoxification; not during acute flares without supervision.
– **Aloe Vera (Aloe barbadensis)**: Soothes mucous membranes and reduces Pitta-aggravated inflammation.
– **Mechanism**: Cooling effect calms digestive fire and promotes tissue healing.
– **Dose**: 15-30 ml of fresh gel or juice daily, diluted in water.
– **Guidelines**: Use inner gel only; avoid if prone to loose stools.
– **Amla (Emblica officinalis, Indian Gooseberry)**: Rich in vitamin C and antioxidants, it repairs damaged tissues and reduces inflammation.
– **Mechanism**: Enhances immunity and detoxifies, supporting pancreatic recovery.
– **Dose**: 1-2 fresh fruits or 500 mg powder daily.
– **Guidelines**: Incorporate in diet or as Chyawanprash.
– **Yashtimadhu (Glycyrrhiza glabra, Licorice)**: Protects gastrointestinal lining and soothes inflammation.
– **Mechanism**: Demulcent properties reduce Pitta and prevent further pancreatic irritation.
– **Dose**: 250-500 mg powder or tea twice daily.
– **Guidelines**: Limit to 4-6 weeks; monitor blood pressure.
– **Ginger (Zingiber officinale)**: Stimulates digestion without overheating, reducing nausea and inflammation.
– **Mechanism**: Anti-inflammatory gingerols improve circulation and Agni.
– **Dose**: 1-2 teaspoons fresh juice or 500 mg capsules daily.
– **Guidelines**: Use dried for Vata balance; fresh for Pitta.
Other supportive herbs include Kutki (Picrorhiza kurroa) for Pitta detoxification, Shatavari (Asparagus racemosus) for tissue rejuvenation, and Ashwagandha (Withania somnifera) for stress reduction, which indirectly aids inflammation control.
Ayurvedic Medications (Formulations)
These herbo-mineral preparations are often prescribed in clinical settings for pancreatitis:
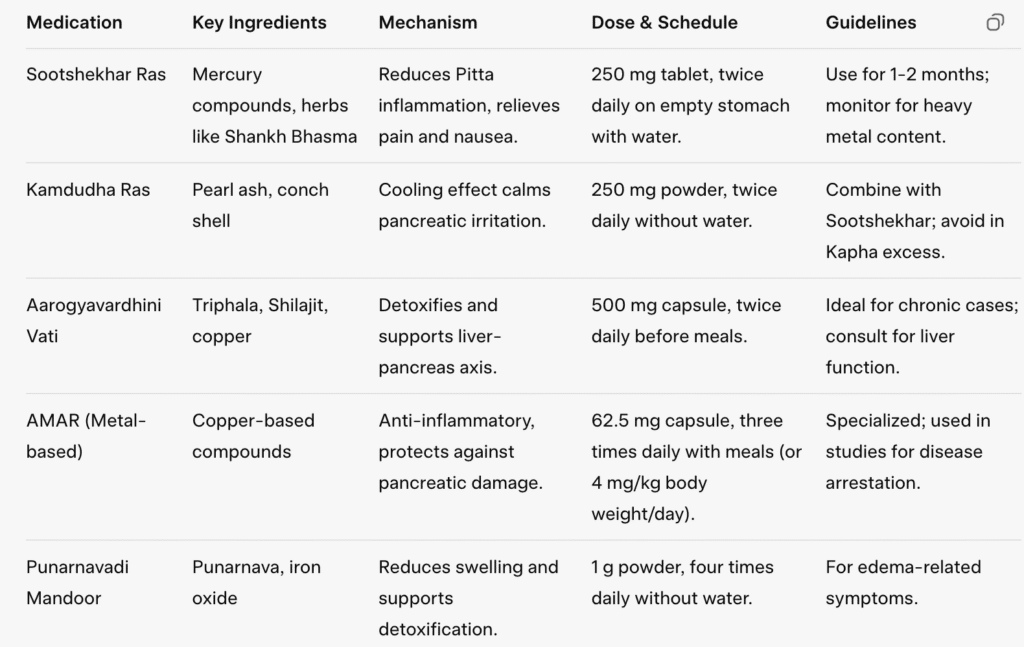
Doses are general and from case studies; actual prescriptions vary. Heavy metal formulations require expert supervision to avoid toxicity.
Dietary Guidelines in Ayurveda for Pancreatitis
Diet (Aahar) is pivotal in Ayurveda for managing pancreatitis, emphasizing Pitta-pacifying, easily digestible foods to reduce inflammation and support Agni. Aim for 1600-2200 calories daily, divided into small, frequent meals.
Foods to Eat
Focus on cooling, Satvik (pure) foods that are cooked, light, and nourishing:
– **Grains**: Rice, barley, wheat, millet (e.g., khichdi with moong dal).
– **Legumes**: Moong dal (green gram), lentils in moderation.
– **Vegetables**: Boiled or steamed bottle gourd, zucchini, pumpkin, leafy greens, cucumbers.
– **Fruits**: Pomegranate, apple, ripe banana, melon, Indian gooseberry (amla).
– **Dairy**: Ghee in small amounts, warm milk with turmeric or cardamom, diluted buttermilk (lassi with cumin).
– **Others**: Herbal teas (fennel, coriander, mint, licorice), soups, fresh juices, roasted puffed rice.
– **Sample Meals**: Breakfast – Rice porridge with ghee; Lunch – Moong dal khichdi with vegetables; Dinner – Light vegetable soup.
These foods soothe the pancreas, promote hydration, and prevent toxin buildup.
Foods to Avoid
Steer clear of Pitta-aggravating items that strain the pancreas:
– Spicy, oily, fried foods (e.g., chilies, deep-fried snacks).
– Alcohol, caffeine, and carbonated drinks.
– Processed, refined, or canned foods (e.g., refined sugar, flour).
– Acidic foods (e.g., citrus, vinegar, pickles, tomatoes).
– Heavy or raw foods (e.g., meat, fish, cheese, raw onions/garlic, cruciferous veggies like broccoli).
– Sour or pungent tastes (e.g., lemon, curd alone, fast food).
Avoid daytime sleeping, heavy dinners, and irregular eating to maintain digestive balance.
Conclusion
Ayurveda provides a comprehensive framework for managing pancreatitis by targeting inflammation through Pitta-balancing herbs like turmeric and guduchi, formulations such as Sootshekhar Ras, and a cooling, digestible diet. Clinical observations suggest these approaches can reduce symptoms, arrest progression, and improve quality of life, especially in chronic cases. However, efficacy varies by individual, and integration with modern care is essential. Lifestyle additions like yoga (e.g., Bhujangasana), meditation, and gentle exercise enhance outcomes. Seek professional guidance to tailor treatments and monitor progress. This information is for educational purposes and not medical advice.



We’re often told: redesign your lifestyle, eat better, manage stress; the perfect recipe for good health.
But is that it? Utterly wrong!
We conveniently ignore a fundamental truth:
“Every emotion sets off a biochemical ripple, shaping the health of our body.”
Dissect ‘stress’ and you’ll find it is never just one thing; it’s layered emotions echoing through the body until they surface as illness.
Until we give this aspect of wellbeing its due attention… until we learn to channel emotional energy consciously… every remedy, every effort will be a surface level fix. This needs unbiased and profound inner work.